What is coronary artery disease?
Coronary artery disease (CAD) is the most common type of heart disease . It is sometimes called coronary heart disease or ischemic heart disease.
For some people, the first sign of CAD is a heart attack. You and your health care team may be able to help reduce your risk for CAD.
Treatment
Treatment for coronary artery disease usually involves lifestyle changes and, if necessary, drugs and certain medical procedures.
Lifestyle changes
Making a commitment to the following healthy lifestyle changes can go a long way toward promoting healthier arteries:
- Quit smoking.
- Eat healthy foods.
- Exercise regularly.
- Lose excess weight.
- Reduce stress.
Drugs
Various drugs can be used to treat coronary artery disease, including:
- Cholesterol-modifying medications. These medications reduce (or modify) the primary material that deposits on the coronary arteries. As a result, cholesterol levels — especially low-density lipoprotein (LDL, or the “bad”) cholesterol — decrease. Your doctor can choose from a range of medications, including statins, niacin, fibrates and bile acid sequestrants.
- Aspirin. Your doctor may recommend taking a daily aspirin or other blood thinner. This can reduce the tendency of your blood to clot, which may help prevent obstruction of your coronary arteries.If you’ve had a heart attack, aspirin can help prevent future attacks. But aspirin can be dangerous if you have a bleeding disorder or you’re already taking another blood thinner, so ask your doctor before taking it.
- Beta blockers. These drugs slow your heart rate and decrease your blood pressure, which decreases your heart’s demand for oxygen. If you’ve had a heart attack, beta blockers reduce the risk of future attacks.
- Calcium channel blockers. These drugs may be used with beta blockers if beta blockers alone aren’t effective or instead of beta blockers if you’re not able to take them. These drugs can help improve symptoms of chest pain.
- Ranolazine. This medication may help people with chest pain (angina). It may be prescribed with a beta blocker or instead of a beta blocker if you can’t take it.
- Nitroglycerin. Nitroglycerin tablets, sprays and patches can control chest pain by temporarily dilating your coronary arteries and reducing your heart’s demand for blood.
Procedures to restore and improve blood flow
Sometimes more aggressive treatment is needed. Here are some options:
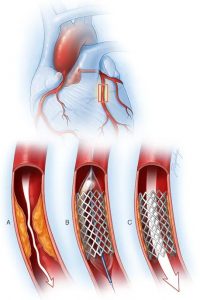
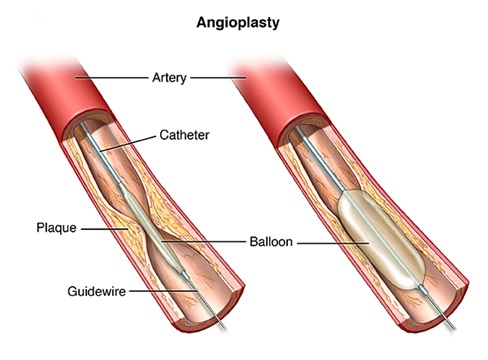
Angioplasty and stent placement (percutaneous coronary revascularization)
Your doctor inserts a long, thin tube (catheter) into the narrowed part of your artery. A wire with a deflated balloon is passed through the catheter to the narrowed area. The balloon is then inflated, compressing the deposits against your artery walls.
A stent is often left in the artery to help keep the artery open. Most stents slowly release medication to help keep the arteries open.
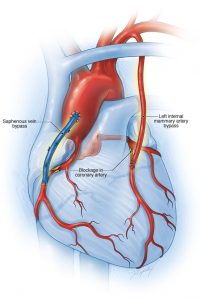
Coronary Artery Bypass Surgery
A surgeon creates a graft to bypass blocked coronary arteries using a vessel from another part of your body. This allows blood to flow around the blocked or narrowed coronary artery. Because this requires open-heart surgery, it’s most often reserved for people who have multiple narrowed coronary arteries.
Coronary artery stent
Coronary bypass surgery
Coronary Angioplasty
A coronary angioplasty is a procedure used to widen blocked or narrowed coronary arteries (the main blood vessels supplying the heart).
The term “angioplasty” means using a balloon to stretch open a narrowed or blocked artery. However, most modern angioplasty procedures also involve inserting a short wire-mesh tube, called a stent, into the artery during the procedure. The stent is left in place permanently to allow blood to flow more freely.
Coronary angioplasty is sometimes known as percutaneous transluminal coronary angioplasty (PTCA). The combination of coronary angioplasty with stenting is usually referred to as percutaneous coronary intervention (PCI).
What is Stenting procedures?
A stent is a tiny tube that your doctor can insert into a blocked passageway to keep it open. The stent restores the flow of blood or other fluids, depending on where it’s placed. Stents are made of either metal or plastic. Stent grafts are larger stents used for larger arteries.
Types of Stents
Currently, there are three types of stents available and commonly called heart stents or cardiac or coronary stents. They are implanted in the narrowed coronary arteries through a procedure called angioplasty or PCI.
- Drug-Eluting Stent (DES)
- Bioresorbable Vascular Scaffold (BVS)
- Bare Metal Stent (BMS)
Benefits of Stenting
Treating blocked arteries with angioplasty and stenting:
- can save your life and reduce heart muscle damage during a heart attack by restoring blood flow to the heart
- may immediately relieve or at least reduce symptoms, such as chest pain, shortness of breath and fatigue, making you feel better and able to do more each day
- can reduce the risk of stroke
- can improve functioning of the kidneys
- can restore blood flow to the legs to prevent gangrene and eliminate the need for amputation
Some patients with blockage in their heart arteries clearly benefit more from open-heart surgery to restore blood flow to the heart. These patients have extensive blockage in all three major arteries or in an artery called the “left main.” In comparison to open-heart surgery, angioplasty and stenting is less invasive than surgery because the clogged or blocked artery is accessed from a tiny incision in the upper leg or the wrist. Angioplasty and stenting may allow you to recover more quickly than you would from surgery, which can also mean less time in the hospital and returning to your regular activities more quickly.
Precautions for Coronary Angioplasty
- Quit smoking.
- Lower your cholesterol levels.
- Eat a healthy diet that is low in saturated fat.
- Maintain a healthy weight.
- Control other conditions, such as diabetes and high blood pressure.
- Get regular exercise.
- Take medications as prescribed by your doctor.
After having a planned (non-emergency) coronary angioplasty, you’ll normally be able to leave hospital the same day or following day. Arrange for someone to take you home.
Before you leave hospital, you should be given advice on:
- any medication you need to take (see below)
- improving your diet and lifestyle
- wound care and hygiene advice during your recovery
You may also be given a date for a follow-up appointment to check on your progress.
You may have a bruise under the skin where the catheter was inserted. This isn’t serious, but it may be sore for a few days. Occasionally, the wound can become infected. Keep an eye on it to check it’s healing properly.
Your chest may also feel tender after the procedure, but this is normal and usually passes in a few days.
